Age related macular degeneration (ARMD)
Age related macular degeneration (ARMD)
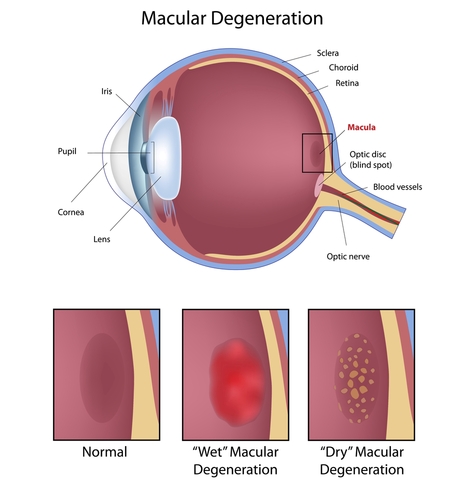


What are the different types of ARMD?
Fortunately dry ARMD is not as aggressive as wet ARMD, although currently there is no effective treatment to halt or reverse these dry changes. Dry ARMD can change and become the wet form. Wet macular degeneration affects only about 10- 15% of people who have ARMD but it accounts for two-thirds of the people who have significant visual loss.
The dry form tends to be slowly progressive and although there is no specific treatment of dry ARMD, only 10% of those registered blind from ARMD are due to the dry type whilst the wet form is responsible for the other 90% of those. Prognosis is therefore worse in the wet form. Prompt assessment is therefore essential for quick diagnosis and treatment if appropriate. Wet ARMD is mainly diagnosed through non-invasive technology using a scanner (Fig e1) and clinical examination. We may also decide to perform a fluorescein angiogram (dye injected through a peripheral venous line) to confirm diagnosis and see the abnormal vessels in the retina.
Recently a new dye less and non invasive technology has been developed, known as OCT angioghraphy, whereby blood vessels in the retina and choroid can be visualised in a 3 dimensional setting. More experience is required with this exciting technology before fluorescein angiography is eventually replaced.

What are the symptoms of macular degeneration?
- Painless and constant blurring of central vision for far and near vision
- Gaps or black spots in the central visual field
- Distortion or bending of straight lines
- Loss of ability to discern colours
- Slow recovery to dark after exposure to light
- Loss of contrast sensitivity
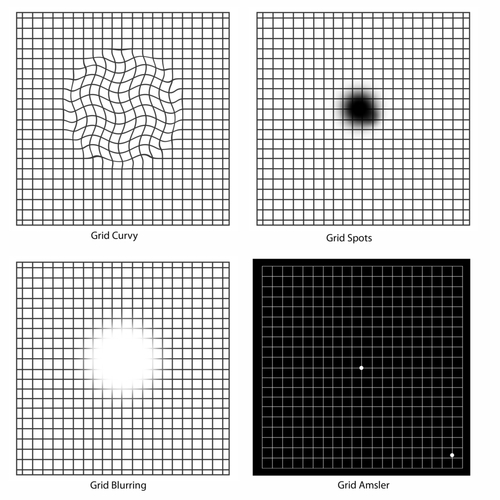
If you have any new symptoms such as those shown here or any change in the straight line you must report this immediately to an ophthalmic health care professional.
What is the treatment for wet ARMD?
Avastin is off label and off license product and is mainly used in those whom National Institute for Health and Clinical Excellence (NICE) has excluded from receiving treatment on NHS as they don’t fulfill the required criteria. These patients may decide to seek treatment privately to prevent further deterioration of vision. Several large randomized controlled trials have indicated that Avastin and Lucentis work with the same efficacy with no significant difference in visual outcome between them. Avastin Is significantly cheaper than Lucentis or Eylea in those whom are funding the treatment themselves and is widely used in Europe and USA with great success.
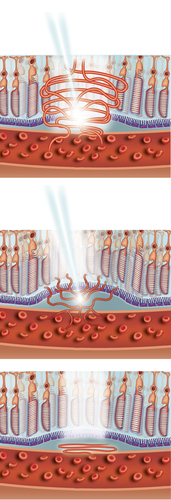
These injections aim primarily to halt progression of abnormal blood vessels and stop the leaking and bleeding in the retina. These drugs prevent significant visual loss in 90% of cases (significant is defined as loss of more than 15 letters in ETDRS charts used in trials) and even improve vision (up to 30%-40%). We expect that for the first 2 years you will be seen in on a regular basis (monthly) though depending on treatment pathway and response these appointments can be decreased in frequency.
It is noteworthy to mention that without anti VEGF injection treatment, the vision can worsen quickly and significant visual loss can ensue within a few weeks to a few months. This reduction can be permanent. Prior to the development of these injections, laser treatment (photodynamic therapy- PDT) had been performed. Trial data suggest that injection are significantly superior to PDT laser although in a very few majority of patients this laser may still have a role. Mr Kashani can discuss with you if this mode of therapy is a viable option for you.
How is the injection given?
What should I expect after an injection?
Take home message is if in doubt please call in and get your symptom checked.
How often will I need treatment and what are the risks?
Like any medical procedure there is a small risk of a complication from Anti VEGF injections.. Here I have listed the main complications from the procedure, although it must be emphasised that such events are unusual and permanent loss of vision as a result of the injection is rare.
Major risks (uncommon)
- Serious eye infection (1 in every 1000 injections)
- Very high pressure in the eye
- Tear or detachment in the retina
- Traumatic cataract
- Blood clots or bleeding inside the eye
- Inflammation in the eye
- Potential for heart attack and/or stroke – only theoretical
Minor risks (common)
- Red eye (bleed at the superficial surface of the eye)
- Sore gritty eye (usually first 48 hours post injection)
- Small specks (floaters ) or transient flashing lights may be seen in your vision for few days
What does the future hold for ARMD?
Current research projects (list not exhaustive)
- Ways of preventing dry turning wet through injections
- Tablets and/or drops for preventing progression of dry ARMD
- Injecting agents to last longer for wet ARMD
- Radiotherapy for wet ARMD
- Reducing invasiveness in treatment of wet ARMD (tablets or drops)
- Stem cell therapy in ARMD
- Telescopic lens placement in advanced ARMD
What do I do if I think I have wet ARMD?
Does NHS provide cover for wet ARMD?
Can I have cataract surgery if I also have ARMD?
What about multivitamins?
Useful websites
NICE – (https://www.nice.org.uk/)
MDS – (http://www.macularsociety.org)
RCO – (http://www.rcophth.ac.uk)
RNIB – (http://www.rnib.org.uk/)
Eastbourne Blind Society – (http://www.eastbourneblindsociety.org.uk/)
NICE website guidance links
https://www.nice.org.uk/guidance/TA294 (Aflibercept)
For more information on Retinal disorders please read the below pages: